HRT Made Easy- A Beginner’s Guide to the Menopause Management
This training covers determining if menopause has started, the drug and non-drug treatment options that help with physical and psychological symptoms, and also it provides clarity on the benefits and risks of taking HRT.
In this training, you’ll learn
1. Diagnosis and management of menopause.
2. Summary of NICE guidance.
3. Principles of hormone replacement therapy.
4.Indications and contraindications for HRT.
5. Management flowchart for patients with menopause.
6. Resources for further study at the end.
Like & Share with your friends 🙂
Watch the Video Now!
Like & Share with your friends 🙂
Thank you for your lovely comments!

![]()
KEY POINTS FROM THE VIDEO TRAINING
Why is it important?
- 45% of women find their menopausal symptoms distressing
- About 20% of symptomatic women will request help
- Women should not feel they have to suffer in silence when menopause is affecting their daily lives at work and at home.
- The effects of menopause are often misunderstood and underestimated — it can impact on health significantly in both the long term and short term.
- Around a million women in the UK use HRT.
- NICE issues first guideline on menopause to stop women suffering in silence. More than a million women could benefit from it.
What do you need to know?
- Menopause is a clinical diagnosis in healthy women over 45 years who have not had a period for at least 12 months and are not using hormonal contraception, or who do not have a uterus and have menopausal symptoms.
- For vasomotor symptoms, offer hormone replacement therapy (HRT) after discussing the short term and longer term benefits and risks.
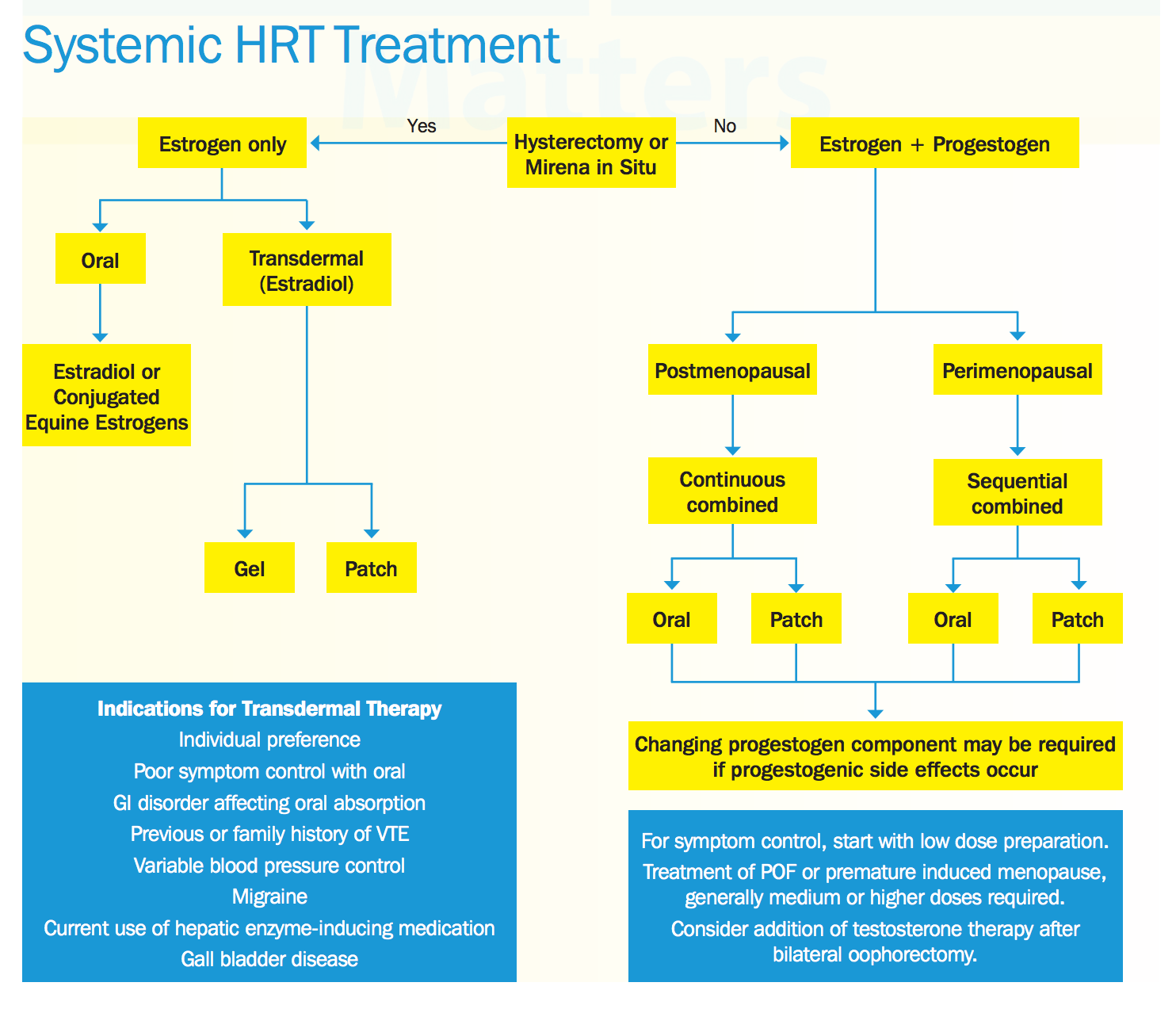
- Prescribe oestrogen and progestogen to women with a uterus, and oestrogen alone to women without a uterus.
- Advise women to report unscheduled vaginal bleeding in the first three months of HRT use (a common side effect) at routine review, but to report such bleeding promptly if it occurs after three months.
Like & Share with your friends 🙂
Ten key points from NICE guideline
(National Institute for Health and Care Excellence – NICE)
- Women should have access to evidence-based information about menopause and treatment options to help them make informed, individual decisions about menopause management
- Blood tests should not be used to diagnose perimenopause or menopause in women aged over 45
- HRT should be offered for menopause-related vasomotor symptoms and low mood
- Clonidine or antidepressants should not be routinely offered for menopausal symptoms
- vaginal oestrogen should be offered for urogenital symptoms, even if HRT is also taken, and continued long term
- Women should have access to specialist services when:
- treatments do not improve menopausal symptoms
- side effects persist
- concern from medical history about the use of HRT
- The decision to stop HRT should be made by each woman when she feels is the right time for her; she should not be given arbitrary limits on the duration of HRT. When stopping HRT can be stopped gradually or suddenly
- HRT does not increase risk of cardiovascular disease when started in women under age 60
- Any increase in breast cancer risk is related to treatment duration and reduces after HRT is stopped, with HRT promoting tumour growth rather than causing tumour
- Women with Premature Ovarian Insufficiency should be offered hormonal treatment up to average age of menopause at least
Initial Consultation
This requires time and should include:
- Current symptoms (need to consider if these symptoms are likely to respond to HRT)
- Menstrual history including last menstrual period, frequency, heaviness and duration of periods, any postmenopausal or post-coital bleeding
- Past medical history and relevant family history – explore risk factors for osteoporosis, breast cancer and coronary heart disease
- Assess woman’s knowledge and expectations
- Lifestyle advice particularly smoking, alcohol, exercise, diet
-
- Teach breast awareness
- Balanced counselling with regard to HRT explaining the risks and benefits
- Patient information leaflets
- Prescribe three months of HRT
- Contact telephone number
Like & Share with your friends 🙂
Investigations
- Blood Pressure as a baseline
- Body mass index as a baseline
- Check entry into breast screening programme, if over 50 years old
- Cervical cytology, if indicated by cervical screening programme
- Pelvic examination, only if symptoms are present
- Full blood count, thyroid function, lipid profile etc. depending on the presenting history or symptoms

Diagnosing the Menopause
The diagnosis of menopause should be based on the woman’s symptoms and age, without relying on laboratory investigations.
Diagnose the following without laboratory tests in otherwise healthy women aged over 45 years with menopausal symptoms:
- Perimenopause — if the woman has vasomotor symptoms and irregular periods.
- Menopause — if the women has not had a period for at least 12 months.
- Menopause — based on symptoms in women without a uterus.
Diagnosis of menopause is usually based on clinical assessment
Blood tests:
- There is little place for the routine measurement of FSH, LH or estradiol
- FSH is commonly measured to ‘detect’ the menopause but is not very reliable, particularly in women under 45 years
- There is no specific biological marker for the menopause
- Women may suffer from vasomotor symptoms but have normal blood test results
- It may be useful to check FSH in women under 45 with atypical symptoms, women complaining of menopausal symptoms using progestogen-only contraception/after a hysterectomy with conservation of ovaries
If FSH is measured;
- Blood should be taken within the first 3 days of the menstrual cycle or two weeks apart if amenorrhoeic
- Serum estradiol levels may be useful in ‘symptomatic’ patients using non oral therapy
Managing the Menopause
How should we assess a woman going through the menopause?
- Assess her symptoms and their severity. This helps determine:
- The most suitable treatment (hormonal, non-hormonal, or non-pharmacological).
- The severity of the symptoms and the extent to which they are affecting the woman’s quality of life.
- Assess her risk of cardiovascular disease (CVD): Women with, or at increased risk of, CVD should have their cardiovascular risk factors managed.
- Assess her risk of osteoporosis.
Discuss the woman’s expectations:
Ask why she has consulted
For example, concern regarding the cause of the symptoms.
Ask if she would like treatment for her symptoms.
Investigations and examinations are not routinely indicated before starting hormone replacement therapy.
- If there is a sudden change in menstrual pattern, intermenstrual bleeding, postcoital bleeding, or postmenopausal bleeding — arrange an urgent 2-week referral if a gynaecological cancer is suspected.
- If there is a personal or family history of venous thromboembolism — consider arranging a thrombophilia screen, bearing in mind that a negative thrombophilia screen does not mean the woman is not at risk.
- If there is a high risk of breast cancer — consider referring for mammography. For more information: NICE guidelines on Early and locally advanced breast cancer and Familial breast cancer.
- If the woman has arterial disease or other risk markers for arterial disease — a lipid profile may be useful.
- If the woman has history, symptoms, or family history of gynaecological disease — consider a pelvic examination.
Like & Share with your friends 🙂
Information and Advice
Give appropriate information to menopausal women and/or their family or carers that includes:
An explanation of the stages of menopause.
The common symptoms of the menopause.
Available treatments for menopausal symptoms, including hormone replacement therapy (HRT), non-hormonal treatments (such as antidepressants), and non-pharmacological treatments (such as cognitive behavioural therapy [CBT] and relaxation techniques).
The risks, possible adverse effects, benefits, and expected duration of treatment with HRT.
Advice on bone health (especially for women diagnosed with premature menopause). For more information, see the Prodigy topic on Osteoporosis – prevention of fragility fractures.
Advice on the importance of keeping up to date with nationally recommended health screening, including:
The NHS Breast Screening Programme that is offered every 3 years to women aged 50 years or over.
The Cervical Screening Programme which is available for all women aged 25 years and over with a frequency of routine 3-yearly recall between 25–49 years of age, then 5-yearly recall until aged 65 years.
Advice on contraception, including that HRT does not provide contraception and that a woman is considered potentially fertile for 2 years after her last menstrual period if she is younger than 50 years of age, and for 1 year if she is over 50 years of age.
Give advise on lifestyle modifications to reduce menopausal symptoms.
For example:
Hot flushes and night sweats — regular exercise, weight loss (if applicable), wearing lighter clothing, sleeping in a cooler room, reducing stress, and avoiding possible triggers (such as spicy foods, caffeine, smoking, and alcohol).
Sleep disturbances — avoiding exercise late in the day and maintaining a regular bedtime.
Mood and anxiety disturbances — adequate sleep, regular physical activity, and relaxation exercises.
Cognitive symptoms — exercise and good sleep hygiene.
Indications for HRT
HRT is indicated:
– For the management of menopausal vasomotor and urogenital symptoms.
77% reduction in vasomotor symptoms compared to placebo in clinical trials
– for women with an early menopause (below 45 years) to prevent osteoporosis, and should normally be continued until the average age of the menopause (52 years)
– for prevention and treatment of osteoporosis in women over 50 years, with menopausal symptoms
Contraindications for HRT
The following situations are absolute contraindications to the prescribing of HRT:
– history of Breast cancer
– active endometrial cancer
– active venous thromboembolism
– active cardiovascular disease
– undiagnosed vaginal bleeding
– uncontrolled hypertension
Extra caution should be exercised in the following situations and advice sought from local specialists:
– previous venous thromboembolism
– previous cardiovascular disease
– endometrial cancer or other oestrogen dependent cancers
– active liver disease
Women taking HRT, who undergo elective surgery should discuss the continuation of their medication with their surgeon.
Most surgeons would advise that HRT can be continued but such women may require VTE prophylaxis.
Managing the Menopause with HRT
If a woman chooses to use hormone replacement therapy (HRT), following a discussion on the risks, possible adverse effects, and benefits, and there are no contraindications to its use:
Advise on lifestyle modifications to reduce menopausal symptoms.
Prescribe the most suitable type of HRT based on her symptoms:
Credit: From menopausematters.co.uk
For vasomotor symptoms:
In a woman with a uterus, offer an oral or transdermal combined (oestradiol plus progestogen) HRT preparation.
In women without a uterus, offer an oral or transdermal oestrogen-only preparation.
In women diagnosed with premature menopause, offer sex steroid replacement with a choice of HRT or a combined oral contraceptive (unless contraindicated, for example in women with hormone-sensitive cancer).
For effects on mood:
Offer a choice of oral or transdermal HRT preparations as above. Consider referring the woman for a trial of cognitive behavioural therapy (CBT) to alleviate low mood and anxiety.
For urogenital symptoms:
Manage according to the specific symptom:
For women with urogenital atrophy (including those already using systemic HRT), offer low-dose vaginal oestrogen. Continue treatment for as long as needed to relieve symptoms.
For women with vaginal dryness, advise that moisturisers and lubricants can be used alone or in addition to vaginal oestrogen.
For sexual dysfunction:
Seek specialist advice regarding the use of testosterone supplementation (off-label use).
Obtain (and document) informed consent before prescribing testosterone for this indication.
For women considering complementary therapies, explain that the quality, purity, and constituents of these products may be unknown.
Although there is some evidence that isoflavones and black cohosh may relieve vasomotor symptoms, their safety is unknown and different preparations may vary.
Advise women with premature menopause that they should not use HRT as a contraceptive.
Hormone Replacement Therapy (HRT) – Example Products

Hormone Replacement Therapy (HRT) – Example Products
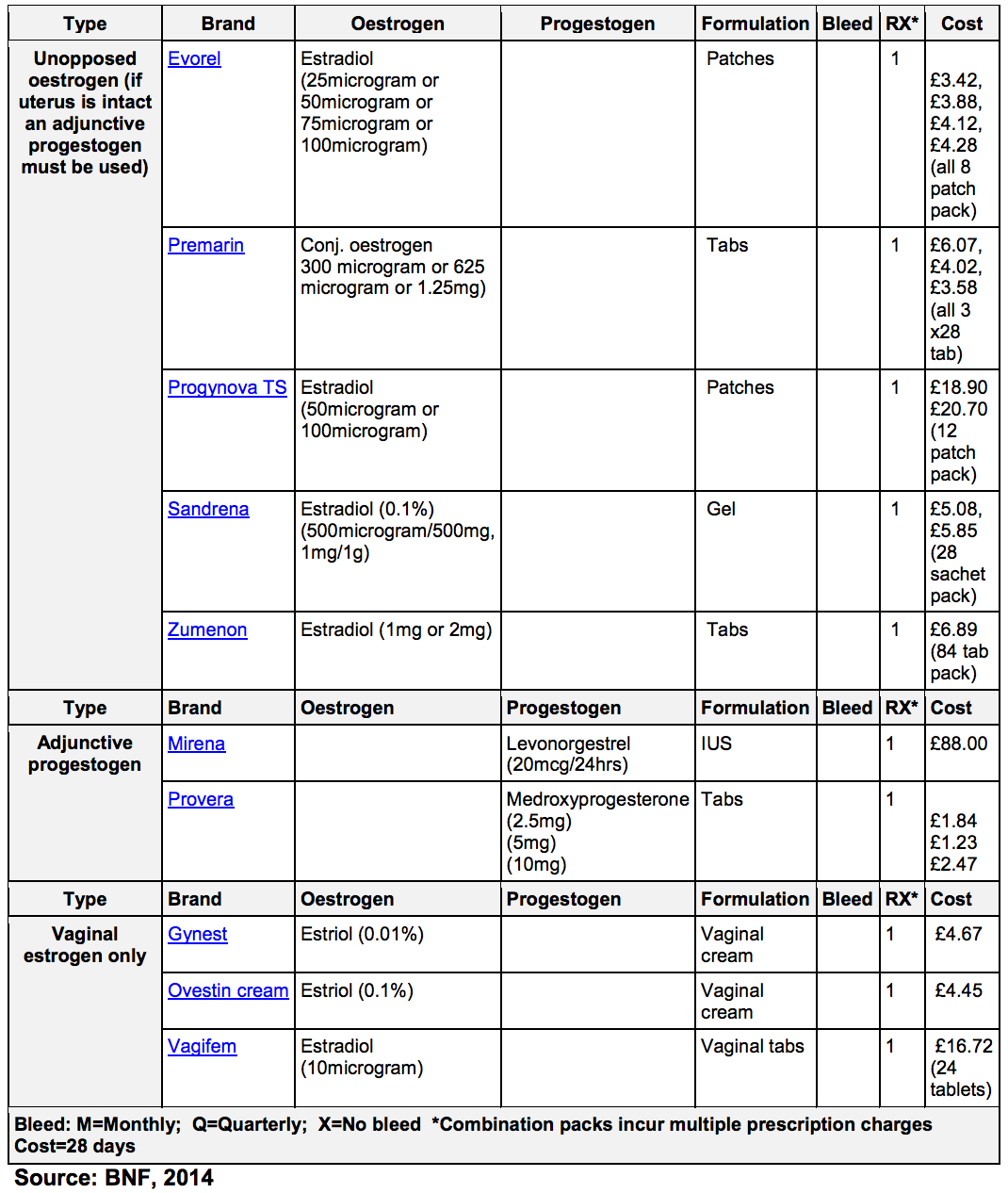
Sequential HRT:
- should be prescribed if a woman’s last menstrual period was less than one year ago
- contains 28 days of continuous estrogen and 10-14 days of progestogen
- should be started at a low dose (containing 1mg estradiol) and increased every 2-3 months until symptoms are controlled
- produces bleeding at a regular, predictable time each month. However, the onset may vary between preparations
- women who are amenorrhoeic using a progestogen-only method need to be informed they are likely to experience a monthly bleed once they commence HRT
Absence of bleeding occurs in approximately 5 % of women and requires no further investigation provided that:
- symptoms are controlled
- the progestogen component is being taken
- there is no irregular bleeding
Minimum daily progestogen doses for a sequential regimen to prevent endometrial hyperplasia are:
- 10 mg dydrogesterone
- 75 μg levonorgestrel
- LNG 52-IUS
- 10 mg medroxyprogesterone acetate
- 0.7 mg norethisterone
- 150 μg norgestrel
- 90 mg progesterone vaginal gel (alternate days)
- 200 mg micronised progesterone
Long cycle HRT:
- contains 70, 2mg estradiol valerate tablets, 14 2mg estradiol valerate and 20 mg medroxyprogesterone acetate tablets as well as 7 placebo tablets
- produces four withdrawal bleeds per year
- may cause initial irregular bleeding in the first two treatment cycles (6 months) but this tends to settle
Endometrial hyperplasia has been reported when lower doses of progestogen are used for 10 days of an 84 day cycle.
Continuous combined HRT:
- contains continuous estrogen and progestogen to induce endometrial atrophy and decrease the risk of endometrial hyperplasia and cancer
- can be prescribed for postmenopausal women to avoid monthly bleeds
- is indicated for women who are 12 months beyond their last natural period or for those with an IUS
Women who start sequential HRT before their periods stop may consider changing to a continuous combined therapy when they are 54 or after four years of taking sequential HRT. Low dose continuous combined HRT (containing 1mg estradiol or 300 micrograms conjugated equine estrogens):
- controls menopausal symptoms
- is bone protective
- gives less erratic bleeding
- results in fewer side-effects than higher dose preparations
Switching from sequential HRT to continuous combined HRT:
- switch at the end of a withdrawal bleed, when the endometrium is at its thinnest
- most women experience some light bleeding/spotting during the first 3-6 months of treatment with more than 75% becoming amenorrhoeic after 6 months use
Tibolone:
- is a selective estrogen receptor modulator
- with estrogenic, progestogenic and androgenic actions
- with the same indications for use as continuous combined HRT
- with the additional effect of improving libido and well-being
ERT (estrogen replacement therapy):
- is for use in women who have had a hysterectomy
Offer advice on stopping HRT:
Explain that:
For vasomotor symptoms, most women require 2–5 years of HRT, but some women may need longer. This judgement should be made on a case-by-case basis with regular attempts to discontinue treatment. Symptoms may recur for a short time after stopping HRT.
Topical (vaginal) oestrogen may be required long term. Regular attempts (at least annually) to stop treatment are usually made. Symptoms may recur once treatment has stopped.
Women with premature menopause usually take HRT up to the average age of the natural menopause (51 years), after which the need for HRT should be reassessed. Some women will still be symptomatic.
Offer women who wish to stop HRT a choice of gradually reducing or immediately stopping treatment.
Explain that:
Gradually reducing or immediately stopping HRT makes no difference to their symptoms in the longer term.
Gradually reducing HRT may limit recurrence of symptoms in the short term.
Symptoms of urogenital atrophy often come back when treatment with vaginal oestrogen is stopped.
Review:
Review the woman at 3 months, then annually thereafter unless there are clinical indications for an earlier review (such as treatment ineffectiveness or adverse effects). At the review:
Assess efficacy and tolerability of treatment(s). If low-dose vaginal oestrogen does not relieve symptoms, consider increasing the dose after seeking specialist advice from a healthcare professional with expertise in menopause.
Reinforce information and lifestyle advice.
If HRT was started in the perimenopause, discuss the option of changing the treatment regimen and/or reducing the dose of oestrogen in the HRT (with longer duration of treatment).
Be aware that HRT may need to be stopped immediately in certain circumstances.
Consider referring the woman to a healthcare professional with expertise in menopause if:
– Treatment is ineffective.
– They have ongoing troublesome adverse effects.
– There are ‘red flag’ symptoms such as unexplained bleeding — arrange an urgent 2-week referral if a gynaecological cancer is suspected.
Further Resources
UK
The guideline, Menopause: diagnosis and management’ is available at
www.nice.org.uk/guidance/NG23.
NICE’s clinical knowledge summary for menopause.
NICE’s information for the public, NHS choices, Women’s Health Concern leaflet to help support women to make informed decisions when advising them about HRT.
http://patient.info/doctor/menopause-and-its-management
http://www.nhs.uk/Conditions/Menopause/Pages/Treatment.aspx
http://www.menopauseacademy.co.uk
Like & Share with your friends 🙂
Patients can also go to NHS Choices for more information. – http://www.nhs.uk/conditions/Hormone-replacement-therapy/Pages/Introduction.aspx
Three PDF format leaflets in- Menopause Matters.co.uk
1. HRT Guide – August 2011. 2 pages (412Kb) – http://www.menopausematters.co.uk/pdf/HRT%20Guide%202016.pdf
2. HRT + You – All you need to know. 48 pages (322Kb)
3. HRT + You – After the first three months. 16 pages (99Kb)
http://www.menopausematters.co.uk/
http://www.womenshealth.gov/publications/our-publications/fact-sheet/menopause-treatment.html
PRIMARY CARE WOMEN’S HEALTH FORUM GUIDELINES –
Menopause Guidelines 2016- pdf – Click Here
Like & Share with your friends 🙂
HRT Guidance and Treatment Pathway
http://www.gwh.nhs.uk/media/163808/wiltshire_hrt_guidance_2014.pdf
Menopause Guidelines
http://www.northoftyneapc.nhs.uk/wp-content/uploads/sites/6/2012/03/Menopause-guideline-Feb-15.pdf
BMJ – http://www.bmj.com/content/351/bmj.h5746
Australia
Management of Menopause toolkit – Click Here
USA
www.womenshealth.gov – fact-sheet- menopause-treatment
Menopause-treatment.pdf – Click Here
Like & Share with your friends 🙂
Sources of advice and support
- The Daisy Network
www.daisynetwork.org.uk - Menopause Matters
www.menopausematters.co.uk - The Menopause Exchange, 0208 420 7245
www.menopause-exchange.co.uk - Fertility Friends
www.fertilityfriends.co.uk - The Infertility Network UK, 0800 008 7464
www.infertilitynetworkuk.com - Women’s Health Concern, 01628 890 199
www.womens-health-concern.org
Like & Share with your friends 🙂
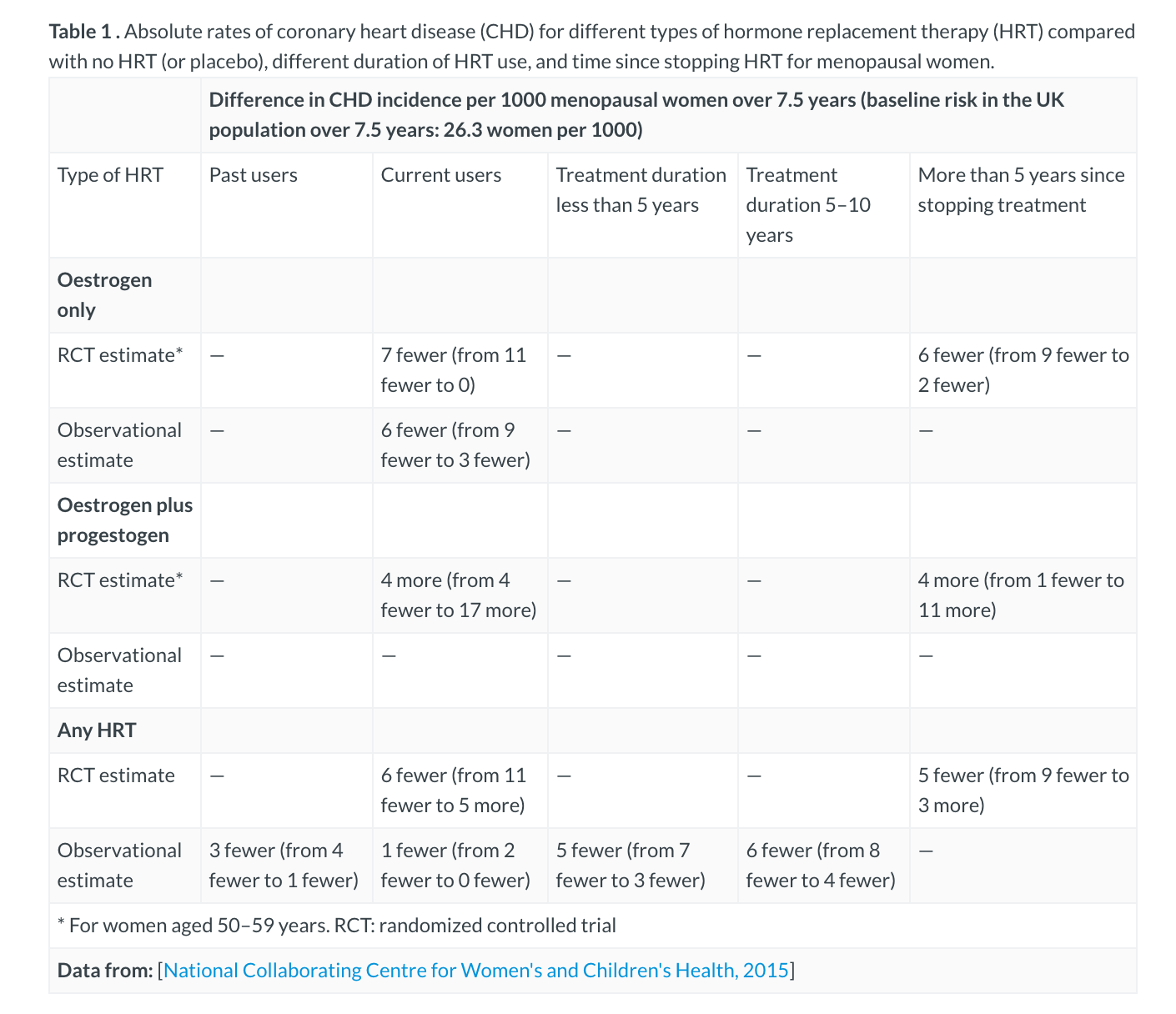
Absolute Rates of CHD
Like & Share with your friends🙂
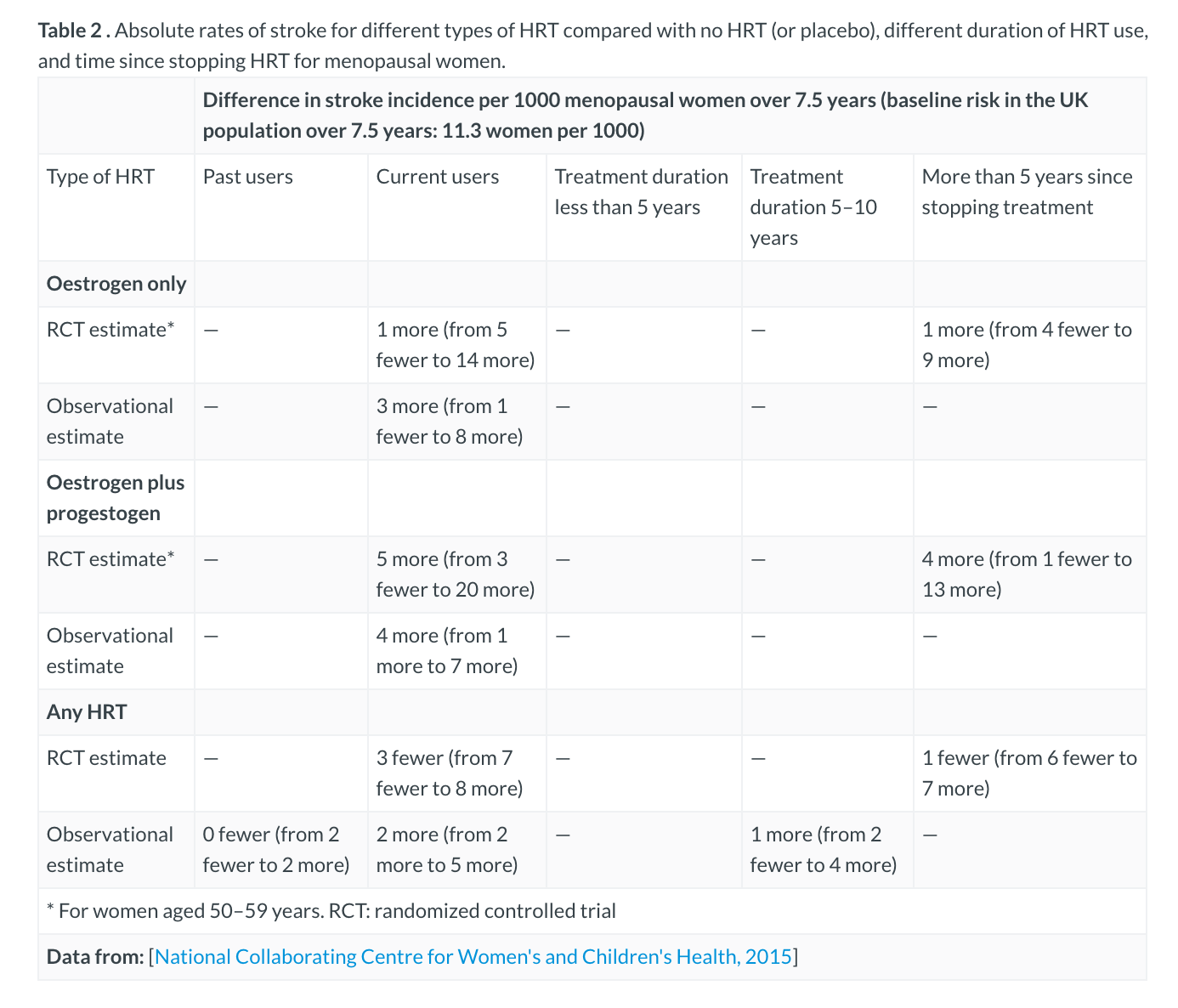
Absolute Rates of Stroke
Like & Share with your friends🙂
Absolute Rates of Breast Cancer

Like & Share with your friends🙂
Absolute Rates of any Fragility Fracture

Like & Share with your friends🙂
Questions that may arise about menopause
These questions may help you be prepared to discuss menopause with patients in simple English.
Diagnosis
- Can you explain more about how menopause is diagnosed?
- Can you diagnose menopause if I am taking a hormonal treatment?
About menopause
- Can you tell me more about menopause and what to expect?
- Should I still use a contraceptive during menopause to avoid pregnancy?
- I am having medical treatment that will trigger menopause: can you explain what I should expect?
About premature menopause (premature ovarian insufficiency)
- Can you explain what causes premature menopause and why it has happened to me?
- Are there any health risks associated with untreated premature menopause?
- What is the likelihood that I could get pregnant after premature menopause?Can you provide any information for my family or carers?Are there any support organisations in my local area?
Lifestyle
- Would it help my menopausal symptoms if I made some changes to my lifestyle, such as becoming more physically active or changing my diet?
- If I am overweight or a smoker does it affect my treatment options?
Treatment for menopausal symptoms
- What types of treatment are suitable for my symptoms?
- What are the benefits and risks of different treatments?
- Are there any complementary therapies that could help?
- I use complementary therapies for my symptoms – are these safe to take alongside other treatments?
- If I already take an antidepressant, will that affect any treatments I can try for mood changes during menopause?
- Can you tell me why you are recommending hormone replacement therapy (HRT)?
- If I don’t want to take HRT, or can’t for medical reasons, what other treatments are there?
- What type of HRT is suitable for me?
- How quickly will HRT improve my symptoms?
- Can I still become pregnant on HRT?
- How and when do we decide I should stop taking HRT?
- Might I have problems when I stop taking HRT?
- Are there any serious side effects from HRT?
- Are there any long-term effects of taking HRT?
- Can you give me some other information (like a leaflet, DVD or a website) about treatment for menopausal symptoms?
For family members, friends or carers
- How can I/we provide help and support?
- Is there any additional support or information that I/we as carer(s) might benefit from?